CAUSES OF INFERTILITY

Female infertility
Ovulation
Without ovulation, there is no conception. The regular monthly menstrual cycles usually coincide with ovulation. Polycystic ovarian syndrome, hypothalamic anovulation, luteal phase insufficiency and problems with thyroid function or prolactin may interfere with ovulation.
Most women will ovulate well into their 40’s and even 50’s but it is the quality of the eggs being released that is thought to be critical.
Young women that do not ovulate regularly can usually be induced to ovulate with either oral or injectable fertility medications.
Ovarian reserve
This is a concept underlying a woman’s reproductive potential, as well as the chances of a healthy and viable pregnancy using her own eggs.
The ovarian reserve is checked using blood tests (FSH, estradiol and AMH tests with samples takes on days 2-5 of the menstrual cycle), as well as an ultrasound to check the ovaries.
Patency
Infection, post-operative scarring or endometriosis, can cause fallopian tubes obstruction.
This prevents egg cells and sperm from getting together and can lead to tubal (ectopic) pregnancy.
Hysterosalpingography is the only non-invasive way to evaluate the patency of the fallopian tubes – that is to determine whether or not the tubes are blocked.
Hydrosalpinx
Hydrosalpinx is the medical term for a fallopian tube that has become filled with fluid due to injury or infection.
The normal function of fallopian tubes is focused on the “conception” of one egg per month as the egg cells is released from the ovary. The Fallopian tubes provide room for the egg and sperm to come together and the means for the fertilized egg to travel to the womb.
Damage to this tiny and delicate passageway can interfere with conception and pregnancy. Hydrosalpinx usually affects both fallopian tubes, (even when only one tube is affected, there is usually some residual damage to the other).
Hydrosalpinges (when both tubes are affected) is a very severe form of tubal damage and pregnancy is usually only achieved with in vitro fertilization.
Uterine and endometrial lining
Fibroids, polyps, intrauterine adhesions from prior surgery, are some of the situations that can cause an abnormal uterus and uterine lining, thus preventing successful implantation of the embryo.
Simple ultrasound imaging can often be sufficient to diagnose any problem.
The REA Hospital can provide hysterosonography (ultrasound following the injection of sterile saline into the womb) or hysteroscopy (surgical procedure to check the interior of the womb) services, which image with higher definition the interior of the womb.
Most of these problems can be solved by surgery.
Genetics
Some patients carry genetic diseases that can cause infertility, such as the Fragile X Syndrome.
Some women (and men) might have chromosomal rearrangements resulting in the presence of abnormal chromosomes in the egg and sperm cells, something that may lead to recurrent miscarriage or infertility.
Even though these problems are thought to be rare, they do exist.
Endometriosis
This is an example of a disease of women of reproductive age that is strongly associated with infertility.
Surgery is the only way to make a definitive diagnosis.
Surgery also contributes significantly to the improvement of pregnancy rates.
50% of women with an endometrioma has infertility issues, while 50% of women with infertility have endometriosis to some extent.
PCOS
Occurring in up to 10 percent of reproductive age women, polycystic ovarian syndrome (PCOS) is a frequently diagnosed disorder of the endocrine system.
In PCOS, women produce high levels of androgens or male hormones (women normally make male hormones, but at a lower level).
This hormonal imbalance interferes with regular ovulation and also results in the presence of multiple immature ova in the ovaries, hence the typical ultrasound image.
Additional symptoms of PCOS may include excess facial or body hair.
Sometimes, lack of regular menstrual cycles is the only symptom.
PCOS is often characterized by insulin resistance, which can lead to long term problems like heart disease, diabetes and high cholesterol.
While there is no cure for PCOS, its symptoms can be managed, enabling women with this condition to have successful pregnancies and good health in the long run.
Fibroids, polyps and uterine disorders
Uterine fibroids
Fibroids of the uterus (leiomyomas or myomas) are benign (non-cancerous) tumors made of smooth muscle that usually grow within the uterine walls.
Fibroids may cause heavy menstrual flow, severe cramping, pelvic pressure and bladder or bowel problems.
Depending on their location, size and growth rate, fibroids can also interfere with conception and pregnancy.
Endometrial polyps
Many women have polyps but may have no symptoms and never know they have them unless they happen to have a pelvic ultrasound.
They are very common in women in their 30’s and 40’s and can probably cause infertility.
Uterine adhesions
Sometimes, particularly after a dilation and curettage procedure, a woman may develop scarring in the uterine cavity.
If severe scarring is present, this is known as Asherman’s syndrome.
This type of scarring may make it difficult or impossible for an embryo to be implanted in the uterus.
Male infertility
Diagnosis and treatment of male infertility
Obstruction
A variety of conditions may prevent potentially normal sperm from traveling from the testes to the ejaculate:
- Ejaculatory duct obstruction
- Congenital absence of the vas deferens (obstructive azoospermia) in which there is normal sperm production in the tests, but no sperm in the ejaculate
- Obstruction may be caused by infection of the epididymis, the part of the male reproductive system where sperm is stored, matures and is transported from the vas deferens to the testes
Treating obstructions:
Sperm flow may be corrected by surgical procedures, such as canalization of the ejaculatory ducts
Other successful treatments for male infertility involve a simple needle aspiration procedure (percutaneous epididymal sperm aspiration or PESA) that will often yield enough sperm to achieve IVF, although usually just enough for one IVF cycle.
Alternatively, a MESA (microsurgical epididymal sperm aspiration) surgery may be performed, yielding many vials of usable sperm.
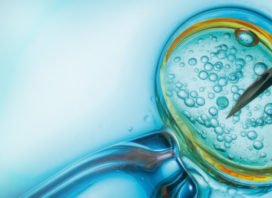
When working with low sperm numbers, whether in the ejaculate or obtained by needle aspiration or biopsy, we consider in vitro fertilization (IVF) with intracytoplasmic sperm injection (ICSI) to be the ideal treatment, a laboratory procedure in which individual sperm cells are injected into an egg, optimizing the possibility of fertilization.
Varicocele
A varicocele is a type of varicose vein in the scrotum.
Due to an otherwise harmless anatomical flaw in the veins which transport blood to and from the testicles, blood flow stops and veins become enlarged and elongated.
The blood carried in these veins may increase scrotal temperature negatively affecting sperm production.
Treating varicocele:
Varicocele may be treated by tying off or ligating the abnormally dilated veins.
This surgery seems to be most effective in men with varicoceles of significant size.
In this surgery, about two thirds of patients will present some improvement in sperm quality.
IVF may also be recommended in this situation.
Non-obstructive azoospermia
Men with very poor sperm production in the testicles and no sperm in the ejaculate often demonstrate high blood FSH levels and, at times, low testosterone levels.
Small testicles and testicular failure are also common.
Testicular biopsy or testicular mapping are diagnostic procedures that evaluate the extent of male infertility by determining if any sperm are being produced at all in the testicles.
Clomid can stimulate the hormones responsible for sperm production.
Sperm counts are re-analyzed 3-6 months after medication is started to evaluate any improvement in sperm production.
Sertoli cell only syndrome:
In this rare male infertility condition, there is complete absence of sperm cells.
For those wishing to have a child, sperm donation is the only recommended option.
Treating non-obstructive azoospermia:
Assuming that the biopsy or mapping have determined that sperm cells are present in the testes, this condition is treated with TESE or testicular biopsy infertility treatment, in which a small sample of tissue from one or both testicles is taken to harvest the sperm for IVF with ICSI treatment.
Depending on the amount of sperm obtained, this treatment can be successful.
Unexplained infertility
This is the diagnosis given when all other test results are normal. For 10-15% of patients, there is no clear answer as to the reason behind their infertility, meaning that the cause may be beyond our current understanding or beyond the sophistication of our testing procedures.
Many couples failing to conceive after 1-2 years of efforts, with all the usual tests coming up normal, may actually have age-related infertility or endometriosis.
On the other hand, there may be other diagnoses or medical problems that we have just not come to understand yet.