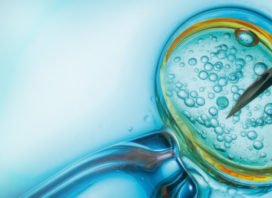
IN VITRO FERTILIZATION

IVF is considered to be one of the most efficient forms of fertility treatment, in that it usually provides the highest rates of successful conception for any one treatment cycle.
For patients with severe male infertility or significantly blocked fallopian tubes, IVF is the only realistic treatment option.
It is often recommended for older patients or when IUI and medications have not been successful.
During the IVF process, a patient’s natural cycle is carefully manipulated through the use of fertility medications.
These medications stimulate the ovaries to produce not one, but a number of mature eggs.
Natural cycle IVF
Natural cycle IVF is when the IVF process is carried out with naturally matured eggs. Without any medication, we avoid the risk of hyperstimulating the ovaries, thus causing them to swell due to the many follicles-eggs. Moreover, the endometrium is not affected by medication and is more amenable to hosting a fertilized egg. At the same time, the female body is generally protected from the high levels of estradiol.
The procedure is simple and egg harvesting can be performed without anesthesia, as the procedure is less invasive. Pregnancy rates after three cycles of NC-IVF approach 50% for women up to 37 years old, and drop to below 25% for women above 38.
Οvarian Sitmulation
In general, ovarian stimulation begins after menstrual bleeding starts. Several similar medications may be used to stimulate follicle development. Τhere are another class of medications used to prevent premature ovulation and, in combination with an antagonist trigger, they may offer protection from severe ovarian hyperstimulation syndrome. They tend to be used for short periods of time in the late stages of ovarian stimulation. There are several different types of stimulation protocols. Although all protocols more-or-less employ the same types of medications, specific protocols may help certain types of patients to have a better response than other types. It is, however, unrealistic to think that switching from one protocol to another will dramatically change a poorly responding patient to a highly responding patient.
IVF with Egg Donation
Sometimes a woman’s eggs are not able to achieve pregnancy. This can be the result of age, illness, genetic abnormalities, prior surgeries, or an unsuccessful response to fertility medications used to stimulate ovulation, or egg production.
Egg donation allows a woman to conceive a child using her own healthy uterus. In this situation, the donated eggs are mixed with sperm and the resulting embryo is implanted into the uterus.
Donor egg IVF is a form of fertility treatment where a young, healthy woman’s eggs are used to produce embryos that are then transferred to the recipient woman’s uterus to establish a pregnancy. The recipient carries the pregnancy to term and gives birth to the baby. BIOMATERNITY’s offers two distinctive egg donor program: the standard
- “Fresh Donor Program” that utilizes fresh donor eggs and the
The initial part of a fresh egg donation IVF cycle is carried out in the same way as for infertility and consists of five basic steps:
- Ripening of the eggs in the donor.
- Retrieval of the eggs in the donor.
- Fertilization of the eggs and growth of the resulting embryos.
- Suppression of the cycle and preparation of the endometrium in the recipient.
- Embryo transfer.
- “Frozen Donor Program” a unique program offering frozen donor eggs.
Oocyte donation is an efficient alternative to using own oocytes in IVF treatment for different indications. Unfortunately, ‘traditional’ (fresh) egg donations are challenged with inefficiency, difficulties of synchronization, very long waiting periods and lack of quarantine measures.
The recent improvements in the efficiency of oocyte cryopreservation, have allowed the option of frozen instead of fresh eggs.
The outcome of using frozen (vitrified) eggs demonstrate that egg cryosurvival is high and that fertilization, embryo development, implantation and pregnancy rates are similar to those reported after fresh egg donation. It also provides additional advantages of being more efficient, more economical, easier for both donors and recipients and potentially also safer, because eggs can now be quarantined for 6 months (or longer) to retest for infectious diseases in the donors.
Egg freezing has improved significantly over the past several years due to fine-tuning of freezing and thawing protocols. Thawed egg survival and viability is much better than it was in the past. These improvements now should allow for reasonable pregnancy and live birth success rates using frozen donor egg.
Egg freezing is far from perfect but using frozen donor eggs instead of fresh donor eggs can have some potential advantages for the recipient couples.
- Synchronization of the cycle between the donor and recipient becomes a non issue.
- There can be a shorter time frame from choosing a donor until having embryo transfer when eggs are already frozen.
- Costs per treatment cycle can be reduced using frozen donor eggs compared to fresh.
- However, the cost per baby born could be lower, the same, or higher – depending on the live birth rate per embryo transfer procedure.
The cost per cycle will certainly be lower with frozen donor eggs. At this time, a reasonable estimate is about 50% for a live birth rate if 2 embryos are transferred after thawing frozen eggs, compared to 85% in our fresh donor egg program when 2 are transferred.
Donor Egg IVF Offers the Best Pregnancy Chances
No fertility treatment offers higher pregnancy chances than egg donation (oocyte donation). The reason is obvious: Egg donors are usually young. An egg donor’s young age means that the recipient’s pregnancy chances and miscarriage risks become those of the young egg donor. Pregnancy chances decline and miscarriage rates rise with advancing female age.
IVF with Sperm Donation
Currently, therapeutic-donor insemination (DI or TDI) is appropriate when the male partner has severe abnormalities in the semen parameters and/or reproductive system.
These abnormalities include both obstructive (caused by a blockage of the ejaculatory ducts) and nonobstructive (due to testicular failure) azoospermia (absence of sperm), which may be congenital or acquired.
Examples of obstructive azoospermia include congenital absence of the vas deferens or previous vasectomy.
Examples of nonobstructive azoospermia include primary testicular failure or secondary testicular failure due to previous radiation treatment or chemotherapy. Severe oligospermia (decreased sperm count) or other significant sperm or seminal fluid abnormalities also are indications for DI. DI also is indicated if the male has ejaculatory dysfunction.
DI may be used if the female is Rh-sensitized and the male partner is Rh-positive
Donor insemination should be considered also in conditions such as:
- where there is a high risk of transmitting a genetic disorder to the offspring,
- where there is a high risk of transmitting infectious disease to the offspring or woman from the man,
- women without a male partner.
IVF with Embryo Donation
One of the most popular methods of Assisted Reproduction Technique is in vitro fertilization (IVF). Frequently there are more embryos created during an IVF treatment than are actually used, thus embryos remain. These embryos are frozen and are a source of hope for others who want to add children to their family.
Embryo adoption or embryo donation is a form of third party reproduction. It is defined as the giving—without compensation—of embryos remaining after one couple’s in vitro fertilisation to either another person or couple for implantation or to research.
Where it is given for the purpose of implantation, the donation is followed by the placement of those embryos into the recipient woman’s uterus to facilitate pregnancy and childbirth in the recipient. The resulting child is considered the child of the woman who carries it and gives birth, and not the child of the donor. This is the same principle as is followed in egg donation or sperm donation.
Most often, the embryos are donated after the woman for whom they were originally created has successfully carried one or more pregnancies to term.